Open Enrollment
Open Enrollment: May 2023
Plan Year: July 1-June 30
WCPS is pleased to continue offering you a comprehensive and affordable health care package. Your Health Care Committee, comprised of A&S, WCESP, WCTA, and WCPS members, works diligently reviewing plans and programs, to recommend improvements while keeping premiums at a minimal cost.
Open Enrollment is a time when you may make any change your benefit elections. Outside of this time, you can only make a change to benefit elections after experiencing a Qualifying Event.
Compliance with Section 125 of the IRS code requires WCPS to follow specific rules regarding timeframes for changes in enrollment.
Annual Open Enrollment
WCPS’s health care plans operate as what’s called Self Insured Plans. This means that while claims are processed through Cigna, WCPS pays for each claim. WCPS wants you to get the treatment that you need when you need it. Our hope is that you seek treatment when you need it in the most appropriate manner.
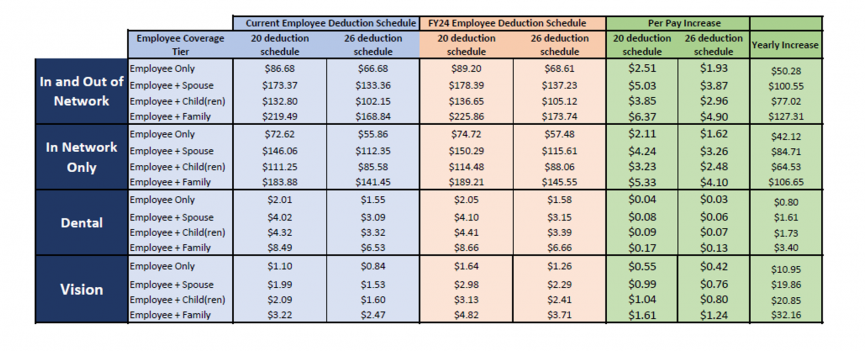
For the FY24 plan year, it is necessary to increase rates with all the plans; medical, dental, and vision. Expenses naturally increase year after year, but we have sustained low or no increases for many years particularly during the pandemic when many people delayed treatment. Please review the chart below to see the rate increases.
- This is the first increase in Medical Premiums in 3 years.
- This is the first increase in Dental Premiums in 10 years.
- This is the first increase in Vision Premiums in over 14 years.
When adding a dependent, you are required to provide documentation within 31 days of the effective date, which is July 1, 2023. Please provide the following via e-mail to [email protected] , pony, or fax at 301-766-8727.
- Adding a spouse > your marriage certificate
- Adding a dependent child > birth certificate
- Medical FSA-used for medical expenses for you and your eligible dependents has increased to $3050
- Dependent FSA-used for childcare has remained at $5000 per year
Qualifying Events
Coverage elections made at Open Enrollment cannot be changed until the next annual Open Enrollment period. The only exception to this IRS Section 125 Rule is if you experience a “Qualifying Event.” A Qualifying Event allows you to make a change to your benefit elections within 31 days of the event. Examples of Qualifying Events include, but are not limited to:
- Marriage
- Divorce
- Birth, adoption, or legal custody of a dependent child
- Involuntary loss of other group insurance coverage
- Death
To Report A Qualifying Event
Log into ESS/Benefits and ‘Report a Life Event’, link in the top right corner. We will contact you when you’re able to change your elections. Submit all required documents to the Benefits Office within 31 days of the event.